Cushing's syndrome Cortisol - and the endocrine system (hypothalamic-pituitary-adrenal (HPA) axis) dysfunction.
Weight Gain and Resistant Hypertension: Causes and Connections to Cortisol Levels
Low ACTH and high cortisol levels often point to Cushing’s syndrome caused by adrenal overproduction, where excess cortisol suppresses ACTH through negative feedback. A similar pattern can also result from long-term corticosteroid use, which reduces ACTH production while maintaining high cortisol levels.
Elevated cortisol, the hallmark of Cushing’s syndrome, can significantly impact the brain, leading to mood changes, cognitive difficulties, and emotional distress. These effects stem both from cortisol’s direct impact on brain function and the psychological strain of managing a chronic illness.
Depression, anxiety, irritability, and rapid mood swings are among the most common psychological manifestations, with some individuals experiencing severe outcomes such as manic episodes, hallucinations, or psychosis.
Cognitive functions are also frequently impaired—many patients report memory problems, difficulty concentrating, and lingering deficits that may persist even after cortisol levels return to normal.
Together, these emotional and cognitive challenges can deeply disrupt daily life, affecting work performance, relationships, and overall quality of sleep and well-being.Causes of Weight Gain and Resistant Hypertension.
Cushing’s Syndrome is a clinical condition caused by prolonged exposure to excessive levels of cortisol. It may result from long-term use of corticosteroid medications, tumors of the adrenal glands or pituitary gland, or, more rarely, ectopic production of adrenocorticotropic hormone (ACTH).
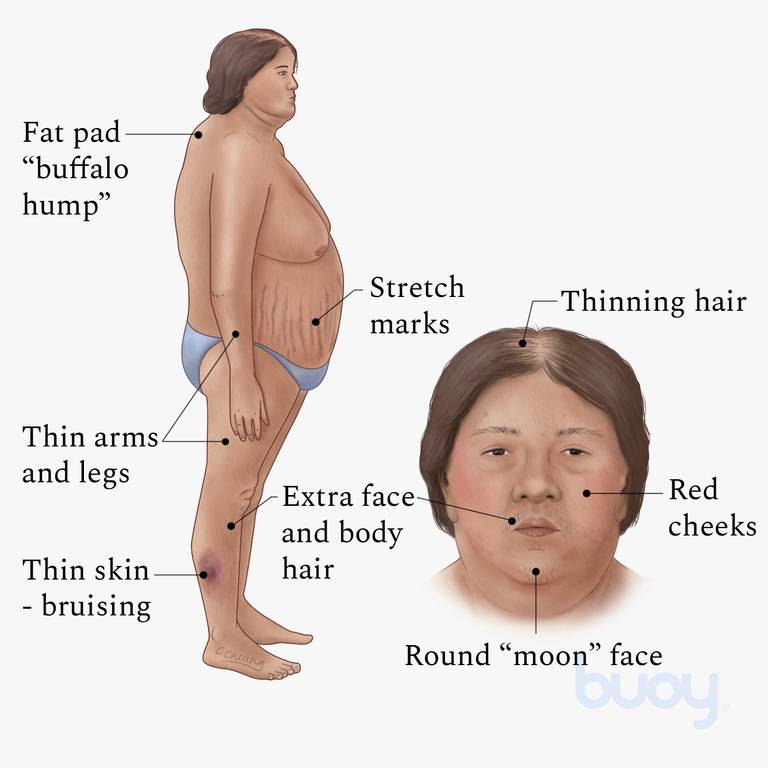
Common symptoms include weight gain, often accompanied by hair loss, difficult-to-control high blood pressure, muscle weakness, thinning of the skin with easy bruising and stretch marks, osteoporosis, mood changes, irregular menstrual cycles, increased thirst and urination, and elevated blood sugar levels.
Cushing's Disease: A specific form of Cushing's syndrome where a pituitary adenoma, a noncancerous tumor on the pituitary gland, makes too much adrenocorticotropic hormone (ACTH). In response, the adrenal glands produce excessive cortisol, disrupting hormone balance and leading to symptoms of Cushing's syndrome. (Reference: OHSU Brain Institute)
Cortisol Levels and Their Impact on Health
High Cortisol Levels: Chronic high cortisol levels, often due to chronic stress or other medical conditions, can cause vascular damage, making individuals irritable and aggressive. Prolonged exposure can lead to psychological symptoms such as euphoria initially, followed by irritability, emotional lability, and depression (Source). Chronic stress and high cortisol can deplete vitamin B6, affecting cognitive function, mood, and physical health.
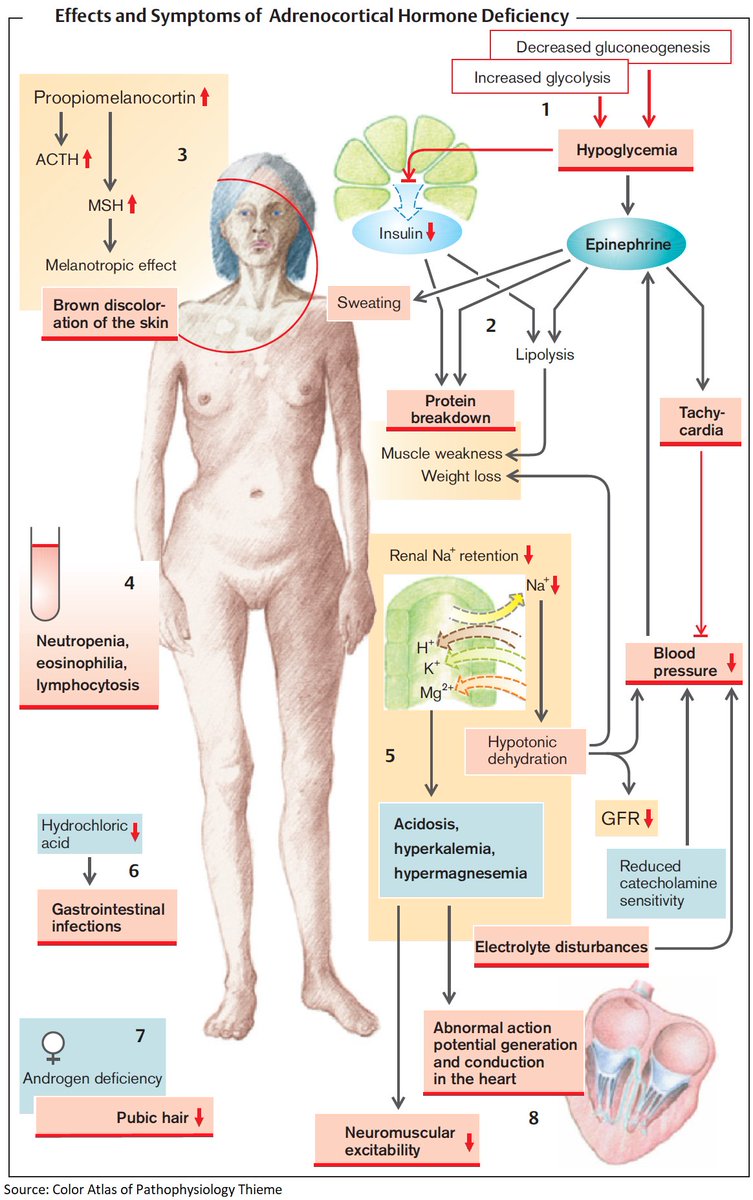
Low Cortisol Levels: Also known as hypocortisolism, low cortisol can result from Addison's disease, an autoimmune disorder, or an underactive pituitary gland. Low cortisol levels cause depression, exhaustion, and a sense of not living. Patients often feel apathetic and depressed (Source).
Behavioral Effects of Cortisol: Elevated cortisol levels are associated with feelings of anger and hostility. Chronic stress leading to high cortisol can exacerbate negative moods (Source). Prolonged exposure to high cortisol can alter immune responses, potentially exacerbating autoimmune conditions.
Cortisol and Fluid Retention
Mechanism of Fluid Retention: Cortisol can cause fluid retention by increasing the reabsorption of sodium and water in the renal tubules, leading to increased fluid volume in the body.
Impact of Excessive Cortisol: Conditions like Cushing's syndrome, which cause elevated cortisol levels, are often associated with fluid retention and edema. Patients undergoing glucocorticoid therapy often experience fluid retention as a side effect.
People with high blood pressure may experience weight gain by this system being more activated.
- High blood pressure itself does not cause obesity but can impact the renin-angiotensin system (RAS). RAS regulates blood pressure and cardiovascular function and, if overactivated, can affect body mass and blood pressure.
Scientific References:
- "Cushing's Syndrome: An Overview of the Therapeutic Approaches": Discusses fluid retention and edema due to excessive cortisol levels.
- "Glucocorticoid Excess and Hypertension: An Update on the Role of the Mineralocorticoid Pathway": Explores effects of glucocorticoids on fluid balance and blood pressure (Reference). Mineralocorticoid Receptor-Mediated Inhibition of the Hypothalamic-Pituitary-Adrenal Axis in Aged Humans
- "Edema and Fluid Retention Associated with the Use of Glucocorticoids": Focuses on mechanisms behind fluid retention and edema.
Hormone Replacement Therapy for Addison's Disease
Corticosteroids: Medicines like Hydrocortisone, prednisone (Rayos), or methylprednisolone (Medrol) are used to replace cortisol. These hormones are administered on a schedule to mimic the body's natural fluctuations in cortisol levels over 24 hours.
Fludrocortisone Acetate: This medication is used to replace aldosterone and help control the amount of sodium and fluids in the body. It works by decreasing the amount of sodium lost in the urine, thus aiding in the treatment of Addison's disease and syndromes where excessive amounts of sodium are lost. (Source)
- Effect on Cortisol Levels: Fludrocortisone significantly decreases maximum adrenocorticotropic hormone (ACTH) and cortisol concentrations. However, ACTH and cortisol values after fludrocortisone are significantly higher in older men compared to younger men. (Source)
Considerations for Patients with Hypocortisolism and ME/CFS or Long COVID
- Exogenous cortisol replacement in patients with ME/CFS or Long COVID and hypocortisolism depends on the case. Chronic corticosteroid use may lead to atrophy of the pituitary and adrenal glands, potentially necessitating lifelong replacement therapy. However, chronic hypocortisolism also favors oxidative stress and chronic inflammation, posing a dilemma that must be assessed between the physician and patient.
Adrenal Insufficiency and Adrenal Burnout
- Adrenal Insufficiency (Addison's Disease): Symptoms include fatigue, muscle weakness, and abdominal pain, often not recognized by doctors. Chronic stress and high cortisol can lead to a state of adrenal exhaustion, described colloquially as adrenal burnout, although this concept is controversial within the medical community.
Medications and Cortisol Levels
- Opioids and Cortisol Assays: Chronic opioid use, including fentanyl, can affect the hypothalamic-pituitary-adrenal (HPA) axis, leading to altered cortisol production or secretion patterns. Opioid-induced adrenal insufficiency (OIAI) can result in symptoms similar to primary adrenal insufficiency, necessitating careful evaluation of cortisol status by healthcare professionals.
Adrenergic and Cholinergic Receptors
- Adrenergic Receptors: Work for the sympathetic nervous system.
- Cholinergic Receptors: Work for the parasympathetic nervous system. (Difference Between Adrenergic and Cholinergic Receptors).
Additional Considerations
- Cortisol on Circadian Rhythm and Cardiovascular System: Cortisol levels influence circadian rhythm and can impact cardiovascular health (Source).
Low cortisol and Addison's crisis is one of the devastating effects and in many cases not recognized by doctors.
Can permanent stress with high cortisol lead to adrenal burnout?
"Adrenal burnout" is not a recognized medical term, but it is often used colloquially to describe a condition known as adrenal fatigue or hypothalamic-pituitary-adrenal (HPA) axis dysfunction. Unfortunately, Adrenal fatigue is a controversial and not universally accepted concept within the medical community even though high level of adrenalin could lead to “adrenal burnout” results.
Behind adrenal fatigue is that chronic stress and high cortisol levels can eventually lead to a state where the adrenal glands become exhausted and are unable to produce adequate levels of cortisol. This, in turn, is believed to result in a range of symptoms such as fatigue, sleep disturbances, mood changes, and other nonspecific complaints.
What are adrenergic and cholinergic?
Difference
Between Adrenergic and Cholinergic Receptors ...
Adrenergic
and cholinergic are two receptors in the autonomic nervous system. Adrenergic
receptors work for the sympathetic nervous system while cholinergic receptors
work for the parasympathetic nervous system.
Adrenergic and Cholinergic Receptors in the Heart
Another
side effect: Cortisol
on Circadian Rhythm
and Its Effect on Cardiovascular System
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7830980/
More information:
https://swaresearch.blogspot.com/2023/09/addisons-disease-vs-cushing-syndrome.html
While opioids can affect the endocrine system, they're generally not known to interfere directly with cortisol assays, which are the tests used to measure cortisol levels in the blood. However, chronic opioid use, including fentanyl, can affect the hypothalamic-pituitary-adrenal (HPA) axis, which may result in altered cortisol production or secretion patterns.
Chronic opioid use can lead to a condition known as opioid-induced adrenal insufficiency (OIAI), where the body's production of cortisol is reduced. This condition can result in symptoms similar to those of primary adrenal insufficiency, such as fatigue, muscle weakness, and abdominal pain.
If someone on long-term opioid therapy like fentanyl has symptoms suggestive of Cushing syndrome or adrenal insufficiency, it is essential to evaluate their cortisol status carefully. This might involve measuring cortisol at different times of the day or after administering synthetic ACTH (adrenocorticotropic hormone) to stimulate cortisol production, known as an ACTH stimulation test.
Furthermore, when assessing cortisol levels, healthcare providers will typically consider the overall clinical context, including medication use, to interpret test results accurately. If there's concern about medication interference with cortisol or other lab tests, alternative testing methods or temporary cessation of the medication under medical supervision might be considered to get accurate measurements.
In any case, this kind of assessment should be done by a healthcare professional, ideally an endocrinologist familiar with the complex interactions between medications like fentanyl and the endocrine system.
References:
Prednisone and other corticosteroids
Cushing
syndrome: Old and new genes
https://www.sciencedirect.com/science/article/abs/pii/S1521690X20300452
Understanding
Cortisol and the Adrenal Axis
https://www.youtube.com/watch?v=s8Lm6lFRw9c
Disclaimer: By accessing and reading this blog, you acknowledge that the information provided is for general informational purposes only and does not constitute medical advice, diagnosis, or treatment. The content is intended to address commonly asked questions and is derived from reputable scientific literature. Always consult a qualified healthcare professional for medical concerns or conditions.
© 2025-2030 Sieglinde W. Alexander. All writings by Sieglinde W. Alexander have a fife year copy right. Library of Congress Card Number: LCN 00-192742 ISBN: 0-9703195-0-9


Comments
Post a Comment