Klebsiella or Streptococcus Ear Infection? A Case of Hidden Mastoiditis Uncovered by HRCT
A recent clinical case raises important questions about the origin and diagnosis of chronic ear infections, particularly when they are accompanied by systemic or recurring symptoms that don't obviously point to the ear as the source—often because initial antibiotic treatment temporarily suppresses the signs without addressing the root cause.
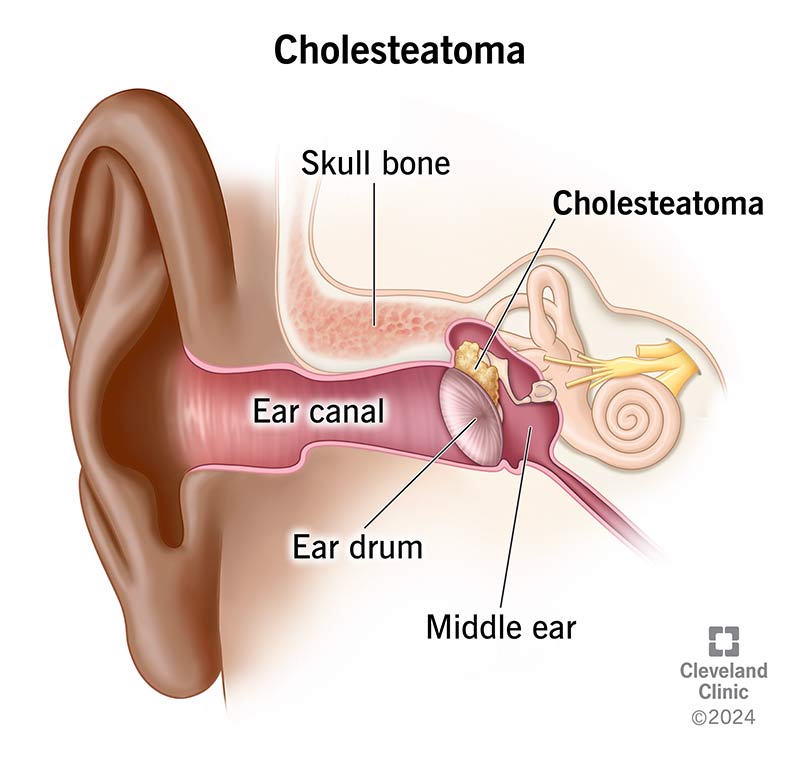 |
| A cholesteatoma in your middle can make you feel dizzy, but the most common symptom is smelly fluid draining from your ear. Credit: https://my.clevelandclinic.org/health/diseases/21535-cholesteatoma |
I was personally drawn to this case because I’ve suffered from frequent ear infections since the age of seven and have been living with tinnitus ever since I contracted COVID-19 in 2020. These experiences have made me keenly aware of how easily ear-related conditions can be overlooked or misinterpreted—especially when their underlying causes remain hidden.
A Mysterious Illness Unfolds
The patient arrived at the hospital with a white blood cell count of 18,460/μL, clearly indicating a serious inflammatory response. While medications managed to bring down the fever, they failed to contain the infection—suggesting that the bacteria might have originated in the upper respiratory tract, a common gateway for pathogens like Streptococcus or Klebsiella.
However, instead of improving, the patient reported feeling cold, exhibited shallow breathing, and had a dangerously low pulse. These are all warning signs of sepsis, a life-threatening condition caused by the body's overwhelming response to infection.
The Limitations of Conventional Imaging
An initial CT scan failed to reveal any abnormalities, yet the patient’s condition continued to deteriorate. Doctors began to suspect that the middle ear infection might not just be a symptom of a larger issue—but possibly the primary source of the systemic infection.
To get a clearer picture, a high-resolution CT scan (HRCT) was ordered—an imaging technique capable of detecting fine structural changes that a standard CT might miss.
A Hidden Infection in the Mastoid
The HRCT finally revealed the culprit: a localized infection in the mastoid, a small, honeycomb-like bone structure located directly behind the ear. This area is filled with tiny air cells and often gets overlooked unless specifically examined.
The scan showed these air spaces were markedly denser, a clear indication of fluid buildup and inflammation. Over time, this untreated infection had led to the formation of a cholesteatoma—an abnormal, cyst-like growth made of skin cells and debris that can erode surrounding bone and harbor bacteria.
This chronic mastoiditis had likely been silently fueling the patient’s repeated ear infections and, worse, had started to spread systemically, threatening other organs or even bones.
Emergency Treatment and Surgery
In response, the medical team acted quickly. The patient was stabilized with intravenous adrenaline, blood pressure-supportive medication, and broad-spectrum antibiotics. Inflammatory markers were still rising, confirming the infection was active and serious.
Thanks to the HRCT, doctors could finally pinpoint the source of the infection. A surgical intervention is now planned to remove the cholesteatoma, stop further spread, and prevent long-term complications.
Key Takeaway
I was personally drawn to this case because I’ve suffered from frequent ear infections since the age of seven and have been living with tinnitus ever since I contracted COVID-19 in 2020. These experiences have made me acutely aware of how easily ear-related conditions can be overlooked or misinterpreted—especially when their underlying causes remain hidden.
A recent clinical case raises important questions about the origin and diagnosis of chronic ear infections, particularly when they are accompanied by systemic or recurring symptoms that don’t obviously point to the ear as the source. This is often due to antibiotic treatments temporarily suppressing symptoms without resolving the actual cause.
Back in 1990, I was diagnosed with a perforated eardrum. The hearing loss developed gradually, so I didn’t notice it for many years. Interestingly, I also experience the opposite at times—a heightened sensitivity to sound, where even normal noises feel uncomfortably loud. This phenomenon is known as hyperacusis.
Reference: https://my.clevelandclinic.org/health/diseases/21535-cholesteatoma
Note: By reading my blog, you acknowledge that I do not provide medical
diagnoses or treatments. The information provided is meant to answer
frequently asked questions and is gathered from reputable scientific
papers.
© 2000-2025 Sieglinde W. Alexander. All writings by Sieglinde W. Alexander have a fife year copy right. Library of Congress Card Number: LCN 00-192742

Comments
Post a Comment