Hypocalcemia (Low Blood Calcium): A Comprehensive Guide to Symptoms, Causes, Diagnosis, and Treatment
Overview
Hypocalcemia refers to an abnormally low concentration of calcium in the blood. Calcium is essential for numerous physiological processes, including muscle contraction, nerve transmission, blood clotting, bone health, and maintaining a steady heartbeat. When calcium levels drop below normal, the nervous and muscular systems can become overly responsive, leading to symptoms ranging from mild tingling in the lips or fingertips to more severe issues such as muscle spasms, seizures, or abnormal heart rhythms.
Autosomal Dominant Hypocalcemia Type 1 (ADH1) is a rare genetic disorder caused by a gain-of-function mutation in the CASR (Calcium-Sensing Receptor) gene. This mutation makes the receptor overly sensitive to calcium, causing it to signal the parathyroid glands to reduce secretion of parathyroid hormone (PTH), despite low calcium levels. This leads to persistent hypocalcemia and excessive loss of calcium in the urine (hypercalciuria).
Autosomal Dominant Hypocalcemia Type 2 (ADH2) is another rare inherited condition, caused by activating mutations in the GNA11 gene. These mutations result in an overactive Gα11 protein, which suppresses the normal signaling pathways that increase blood calcium levels. As a result, individuals experience hypocalcemia with symptoms such as muscle cramps, tingling sensations, and seizures, even when PTH levels are normal or low.
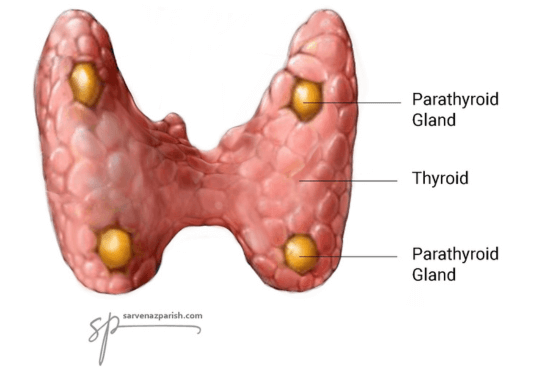
Hypocalcemia can also arise from a range of non-genetic causes, often due to impaired calcium regulation. Common contributors include parathyroid hormone (PTH) deficiency or resistance, vitamin D deficiency, and chronic kidney disease. Other factors may involve acute conditions like pancreatitis, low magnesium or protein levels, malabsorption syndromes, certain medications, or complications following surgeries—especially those involving the thyroid or gastrointestinal tract.
The parathyroid glands, typically four small nodules located on the back of the thyroid gland, play a central role in calcium regulation. These glands continuously monitor blood calcium levels and release PTH when levels fall. PTH is vital for maintaining calcium balance by increasing calcium absorption in the intestines, reducing calcium loss in the urine, and mobilizing calcium from bones.
The underlying mechanisms typically involve:
-
Impaired PTH or vitamin D activity
-
Decreased calcium absorption in the gut
What it is:
- Hypocalcemia: The medical term for low blood calcium.
- Normal Range: Typically 8.5 to 10.2 mg/dL (2.12 to 2.62 mmol/L), but varies by lab.
Symptoms of Hypocalcemia
Mild to Moderate Symptoms
In many cases, especially when hypocalcemia develops slowly, symptoms may be mild or even absent. When present, early symptoms often involve the nervous system, muscles, skin, and psychological health:
Neurological
-
Tingling or numbness (paresthesia) in the lips, tongue, fingers, and feet
-
Lightheadedness or occasional confusion
Musculoskeletal
-
Muscle cramps and spasms, especially in the back, legs, and abdomen
-
Generalized muscle stiffness or aches
-
Involuntary twitching
Skin, Hair, and Nails
-
Dry, scaly skin
-
Brittle nails
-
Coarse hair, especially with long-term deficiency
Psychological
-
Anxiety, irritability, and depression
-
Difficulty concentrating or memory issues
Severe or Acute Symptoms (Tetany and Emergency Features)
When calcium levels fall rapidly or reach critically low levels, the nervous and muscular systems become hyperexcitable, potentially resulting in:
Severe Muscle Spasms
-
Tetany: Sustained muscle contraction causing painful spasms
-
Carpopedal spasms: Characteristic hand and foot contractions, with hands forming a clenched “claw-like” shape
Breathing Issues
-
Laryngospasm: Sudden throat muscle spasms that can cause airway obstruction and breathing difficulty, especially dangerous in children
Cardiac
-
Arrhythmias (abnormal heart rhythms)
-
Prolonged QT interval on ECG
-
Rarely, heart failure
Neurological
-
Seizures
-
Confusion, hallucinations, and cognitive disturbances
Physical Signs Detected on Examination
Doctors may perform specific bedside tests during physical examination:
-
Chvostek’s Sign: Tapping over the facial nerve causes twitching of facial muscles.
-
Trousseau’s Sign: Inflating a blood pressure cuff on the arm induces a hand spasm (carpopedal spasm) due to neuromuscular excitability.
Causes of Hypocalcemia
The causes of hypocalcemia can be diverse, affecting calcium intake, absorption, or regulation.
Common Causes
-
Vitamin D Deficiency: Reduces calcium absorption in the gut. Common in people with little sun exposure, poor diet, or malabsorption disorders.
-
Hypoparathyroidism: Reduced secretion of parathyroid hormone (PTH), often due to thyroid/parathyroid surgery, autoimmune disease, or genetic conditions.
-
Chronic Kidney Disease (CKD): Fails to activate vitamin D (into calcitriol) and disrupts calcium/phosphorus balance.
-
Magnesium Deficiency (Hypomagnesemia): Impairs PTH secretion and action.
Other Significant Causes
-
Acute Pancreatitis: Triggers fat necrosis, binding calcium with fatty acids.
-
Medications:
-
Bisphosphonates (used in osteoporosis)
-
Anticonvulsants
-
Citrate (used in transfusions)
-
-
Malabsorption Syndromes:
-
Celiac disease
-
Gastric bypass surgery
-
-
Poor Dietary Intake: Insufficient calcium or protein
-
Critical Illness: Sepsis, burns, or rhabdomyolysis
-
Hungry Bone Syndrome: After surgery for hyperparathyroidism, bones rapidly absorb calcium.
Genetic and Rare Causes
Pseudohypoparathyroidism (PHP)
A rare genetic disorder where the body does not respond to PTH, despite high hormone levels.
-
Cause: Mutations in the GNAS gene
-
Biochemical Profile: Low calcium, high phosphorus, high PTH
-
Types:
-
Type 1a: With Albright’s Hereditary Osteodystrophy (AHO) – short stature, round face, obesity, and short fingers
-
Type 1b: PTH resistance only, no physical traits
-
Type 2: Defect in downstream signaling despite normal cAMP response
-
-
Treatment: Requires active vitamin D (calcitriol) and calcium supplementation
Diagnosis of Hypocalcemia
Diagnosis is based on lab tests that measure serum calcium levels and evaluate possible causes.
Primary Lab Tests
-
Total Calcium: Includes both bound and unbound calcium
-
Albumin: Used to correct total calcium level (as calcium binds to albumin)
-
Ionized Calcium: Measures free, active calcium — most accurate for clinical decision-making
Additional Tests
-
Parathyroid Hormone (PTH): Low or high PTH helps differentiate causes
-
Phosphate and Magnesium: High phosphate and low magnesium are often seen in PTH-related causes
-
Vitamin D (25-OH and 1,25(OH)2D): Assesses reserves and activation status
-
Creatinine: Evaluates kidney function
Other Investigations
-
ECG: To detect QT interval prolongation and arrhythmias
-
Bone Density Scans (DEXA): For chronic hypocalcemia cases
-
Urine Tests: To assess calcium and phosphate excretion
Important Note for Testing
Ionized calcium testing requires quick and careful handling of blood samples — use non-heparinized tubes, and analyze promptly to avoid inaccurate results.
Treatment of Hypocalcemia
Emergency Treatment (Severe Hypocalcemia)
Indications
Seizures, tetany, breathing difficulty, or cardiac instability
Interventions
-
IV Calcium Gluconate: Administered slowly under cardiac monitoring
-
Correct Magnesium Deficiency: If present, often with IV magnesium sulfate
-
Monitor ECG, especially in heart disease patients
Chronic or Mild Hypocalcemia
Oral Supplements
-
Calcium Carbonate or Citrate: Best taken between meals for absorption
-
Activated Vitamin D (Calcitriol): Especially in CKD or hypoparathyroidism
Advanced Therapy
-
Synthetic PTH (e.g., PTH 1-84): For chronic hypoparathyroidism when standard treatment fails
Additional Management
-
Medication Review: Stop or adjust drugs causing calcium loss
-
Low-Phosphorus Diet: May be recommended
-
Regular Monitoring: Calcium, phosphorus, magnesium, kidney function
-
Caution with Digoxin: IV calcium must be used carefully to avoid cardiac toxicity
Hypocalcemia in Special Populations
Newborns and Infants
-
Prematurity, low birth weight
-
Maternal diabetes
-
Inborn errors of metabolism
-
Common codes: P71.1 (Other hypocalcemia of the newborn)
ICD-10 Coding for Hypocalcemia
Main Codes (ICD-10-CM, USA)
-
E83.51 – Hypocalcemia (general)
-
E83.50 – Disorders of calcium metabolism, unspecified
-
E58 – Dietary calcium deficiency
-
P71.1 – Other hypocalcemia of the newborn
Note: ICD-10-GM (used in Germany) may vary slightly in code structure but E83.51 is widely accepted.
When to Seek Immediate Medical Attention
Call emergency services or go to the ER if you experience:
-
Seizures
-
Severe muscle cramps or spasms
-
Breathing difficulty
-
Palpitations or chest pain
-
Confusion or hallucinations
Conclusion
Hypocalcemia is a potentially serious condition that affects many systems of the body. While mild forms may go unnoticed, severe deficiency can be life-threatening. Early recognition, proper testing, and individualized treatment—often involving calcium and vitamin D supplementation—can prevent complications. Understanding the underlying cause is crucial for long-term management and prevention of recurrence. If you suspect hypocalcemia or are at risk due to surgery, kidney disease, or vitamin D deficiency, consult your healthcare provider for evaluation and monitoring.
References:
Hypocalcemia: https://my.clevelandclinic.org/health/diseases/23143-hypocalcemia
Hypocalcemia: https://www.ncbi.nlm.nih.gov/books/NBK430912/
Hypocalcemia (Low Level of Calcium in the Blood): https://www.msdmanuals.com/home/hormonal-and-metabolic-disorders/electrolyte-balance/hypocalcemia-low-level-of-calcium-in-the-blood
Hypocalcemia: https://www.ncbi.nlm.nih.gov/books/NBK430912/
https://www.hopkinsmedicine.org/health/conditions-and-diseases/the-parathyroid-glands
https://www.webmd.com/a-to-z-guides/what-is-hypocalcemia
© 2025-2030 Sieglinde W. Alexander. All writings by Sieglinde W. Alexander have a fife year copy right.
Library of Congress Card Number: LCN 00-192742
ISBN: 0-9703195-0-9

Comments
Post a Comment