Muscle Weakness: Causes, Viral Links, and the Physiology Behind Muscle Function
Muscle weakness is a common but complex symptom that can arise from many different systems in the body. It may develop gradually, appear suddenly after an illness, or worsen over time due to genetic, neurological, metabolic, or infectious causes. Understanding why muscles become weak requires understanding how muscles normally work, what they need to function, and how viruses and diseases disrupt these processes.
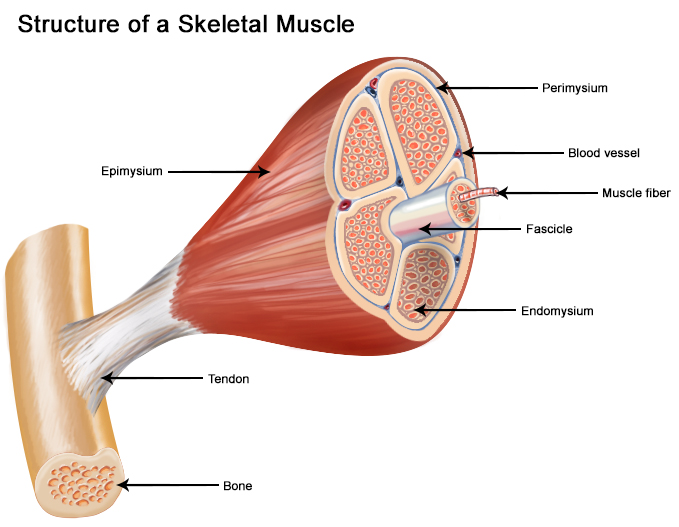
How Muscles Normally Work
For a muscle to contract, relax, and maintain strength, seven essential systems must function together:
Energy + Oxygen + Nerve Signals + Electrolytes + Water + Protein + Blood Supply
A failure in any one of these systems can result in muscle fatigue, pain, or true weakness.
1. Energy (ATP): The Power Source of Muscle
Muscles are powered by adenosine triphosphate (ATP), the primary energy currency of the body.
ATP Production Pathways
-
Aerobic respiration (mitochondria)
Uses oxygen to generate ~30–32 ATP per glucose molecule. -
Anaerobic glycolysis
Rapid ATP production without oxygen (2 ATP per glucose). -
Phosphagen system (creatine phosphate)
Immediate energy for short bursts (<10 seconds). -
Fat metabolism (β-oxidation & ketosis)
Sustained ATP production during prolonged activity.
Scale of ATP Use
-
The body does not store ATP in large amounts.
-
An adult recycles roughly their own body weight in ATP every day.
-
A single muscle cell can use millions of ATP molecules per second.
When ATP production is impaired—due to infection, lack of oxygen, toxins, or metabolic disease—muscle contraction weakens rapidly.
2. Oxygen: Fuel for Efficient Muscle Work
Oxygen allows mitochondria to generate ATP efficiently.
-
Delivered by red blood cells
-
Required for sustained muscle activity
-
Low oxygen causes burning, fatigue, and weakness
Causes of Reduced Oxygen Delivery
-
Anemia
-
Lung disease
-
Circulatory disorders
-
Red blood cell destruction from:
-
Certain viral infections
-
Medications (e.g., penicillin, sulfa drugs, antimalarials, acetaminophen)
-
3. Nervous System Signals: The On–Off Switch
Muscles only contract when they receive electrical signals:
Brain → spinal cord → motor nerve → neuromuscular junction → muscle fiber
If nerve signaling is disrupted:
-
The muscle cannot contract normally
-
Weakness develops even if the muscle itself is healthy
Neuromuscular Diseases That Cause Weakness
-
Amyotrophic lateral sclerosis (ALS)
-
Spinal muscular atrophy
-
Myasthenia gravis
-
Muscular dystrophy
4. Electrolytes: Minerals That Enable Contraction
Electrolytes allow muscles and nerves to generate electrical activity.
-
Calcium (Ca²⁺) – Triggers contraction
Calcium shifts the troponin complex on actin, exposing myosin-binding sites and enabling the power stroke. -
Sodium (Na⁺) & Potassium (K⁺) – Generate nerve impulses
-
Magnesium (Mg²⁺) – Allows muscle relaxation
Imbalances can cause:
-
Weakness
-
Muscle cramps
-
Spasms
-
Paralysis in severe cases
5. Water (Hydration): Structural and Electrical Stability
Muscles are approximately 75% water.
Dehydration:
-
Reduces strength and endurance
-
Impairs coordination
-
Disrupts electrolyte balance
-
Increases injury risk
6. Protein & Amino Acids: Muscle Repair and Growth
Muscle fibers constantly undergo breakdown and repair.
-
Protein is required to rebuild muscle tissue
-
Leucine, a branched-chain amino acid, strongly stimulates muscle protein synthesis
-
Amino acids can also serve as fuel during exercise
Complete Protein Sources
-
Meat, poultry, fish
-
Eggs
-
Dairy
-
Legumes and tofu
Protein deficiency leads to:
-
Muscle wasting
-
Delayed recovery
-
Progressive weakness
7. Blood Supply: Delivery and Waste Removal
The circulatory system:
-
Delivers oxygen, nutrients, and hormones
-
Removes carbon dioxide and lactic acid
Blood transports critical hormones including:
-
Insulin (metabolism)
-
Testosterone & estrogen (muscle mass)
-
Epinephrine & norepinephrine (fight-or-flight)
-
Serotonin (mood and sleep)
Poor circulation results in early fatigue and weakness.

The sarcolemma is the muscle fiber’s plasma membrane. It plays a central role in:
-
Action potential propagation
-
Excitation–contraction coupling
-
Structural integrity during contraction
What Happens When the Sarcolemma Tears?
-
Calcium floods into the muscle cell
-
Cellular enzymes are activated
-
Muscle fibers are damaged and degrade
-
Repeated injury leads to muscle wasting and weakness
Dysfunctional Sarcolemma & Muscular Dystrophy
Duchenne muscular dystrophy
-
Caused by absence of dystrophin
-
Affects mainly males
-
Progressive muscle weakness beginning in childhood
Becker muscular dystrophy
-
Partial dystrophin function
-
Slower progression
Without dystrophin, normal muscle contractions cause repeated membrane tearing, calcium overload, and fiber destruction.
Acute Viral Myositis
A rare acquired skeletal muscle disease characterized by:
-
Sudden onset muscle pain
-
Tenderness
-
Weakness
-
Occurs during or after viral illness
-
Elevated serum creatine kinase (CK)
Most Common Viral Causes
-
Influenza B (most common)
-
Influenza A (less frequent)
Viral myositis most often appears during recovery, not during peak infection.
How Viruses Cause Muscle Weakness
Viruses may:
-
Directly invade muscle fibers
-
Trigger immune-mediated muscle inflammation
-
Disrupt mitochondrial ATP production
-
Damage nerves supplying muscle
-
Cause systemic electrolyte disturbances
The result is painful, weak muscles with preserved reflexes in many cases.
Polio and Muscle Weakness
Poliomyelitis
Polio damages motor neurons in the spinal cord.
Long-Term Effects
-
Persistent muscle weakness
-
Muscle atrophy
-
Weakness may appear years later (post-polio syndrome)
-
Overuse or underuse worsens symptoms
Weakness is most pronounced in muscles that originally lost nerve supply.
Toxins and Metabolic Interference
Certain poisons and drugs impair muscle energy production or nerve signaling.
Examples
-
Cyanide (blocks cellular respiration)
-
Sedatives and hypnotics
-
Antidepressants (SSRIs, SNRIs)
-
Cardiovascular drugs
-
Alcohols
-
Pesticides
-
Envenomations (snakes, spiders, insects)
These substances may cause acute or chronic muscle weakness.
Why Muscle Weakness Occurs: A Unified View
Muscle weakness develops when one or more of the following fails:
-
ATP production
-
Oxygen delivery
-
Nerve signaling
-
Sarcolemma integrity
-
Electrolyte balance
-
Hydration
-
Protein availability
-
Blood circulation
https://pmc.ncbi.nlm.nih.gov/articles/PMC7466328/#:~:text=While%20the%20sensitivity%20of%20assays%20employed%20to,is%20frequently%20tested%20by%20routine%20doping%20controls.
A blood test for ATP levels is possible, typically measuring
intracellular ATP in white blood cells (leukocytes) using a bioluminescence
assay with luciferin-luciferase, revealing cellular energy status for assessing
mitochondrial health, metabolic disorders, or immune function, though it requires
careful sample handling (like using heparinized blood) and is used more in
specialized diagnostics than routine checks.
https://athenslab.gr/en/exetaseis-prolipsis/detoxscan-elegxos-oxeidotikou-stres/atp-intracellular-2408
Conclusion
Muscle weakness is not a single disease, but a sign of disruption across multiple systems. Viral infections—especially influenza and COVID-19—can cause sudden, painful weakness through acute myositis. Genetic disorders like muscular dystrophy weaken muscles by destabilizing the sarcolemma. Neurological diseases impair nerve signaling, while metabolic and circulatory problems starve muscles of energy and oxygen.
For muscles to function well, they require:
Energy + Oxygen + Nerve Signals + Minerals + Water + Protein + Healthy Circulation
Understanding these foundations allows clinicians and patients alike to better recognize, diagnose, and manage muscle weakness—whether it arises from infection, genetics, or systemic disease.
Other readings:
Dysferlin Protein: Key Roles, Genetic Locations
https://swaresearch.blogspot.com/2025/01/dysferlin-protein-key-roles-locations.html
Causes of Weakness in the Teres Minor and
Triceps: The Role of Sarcolemma Dysfunction and ACTN3 Gene Mutations
https://swaresearch.blogspot.com/2025/02/causes-of-weakness-in-teres-minor-and.html
Muscle Integrity, DYSF Methylation, and Immune
Dysfunction: A Molecular Overview of Skeletal, Cardiac, and Smooth Muscle
Vulnerabilities
https://swaresearch.blogspot.com/2025/09/muscle-integrity-dysf-methylation-and.html
Bethlem Myopathy and the Role of the Sarcolemma
https://swaresearch.blogspot.com/2025/02/bethlem-myopathy-and-role-of-sarcolemma.html
© 2025-2030 Sieglinde W. Alexander. All writings by Sieglinde W. Alexander have a fife year copy right. Library of Congress Card Number: LCN 00-192742 ISBN: 0-9703195-0-9

Comments
Post a Comment